Professor Hua Wei: Current situation and challenges of prevention and treatment of sudden cardiac death in China.
introduction
Sudden cardiac death is one of the most important problems faced by cardiologists. In many cases, the success rate of rescue is not high, so the mortality rate is still high. At present, most of the solutions are passive, and ICD (Implantable Defibrillator) is installed after patients survive, but the status quo of diagnosis and treatment of sudden cardiac death (SCD) is not optimistic. In this regard, Fuwai Hospital of China Academy of Medical SciencesProfessor Hua Wei.Report on "Current situation and challenges of prevention and treatment of sudden cardiac death in China".He mentioned that early defibrillation is the key to improve the survival rate of cardiac arrest, and early preventive implantation of ICD is the most effective means to prevent sudden cardiac death.

Sudden cardiac death is the first killer of cardiovascular disease.
The leading cause of death among adults in the United States is SCA (cardiac arrest), with an annual incidence of 450,000, which exceeds the sum of all these diseases, such as stroke (167,366), lung cancer (157,400), breast cancer (40,600) and AIDS(42156).
As a populous country, how many people have sudden cardiac death every year in China? Fuwai Hospital conducted an epidemiological survey more than ten years ago, and included the population of Beijing, Guangzhou, Shanxi and Xinjiang for sampling survey. It was the first time that the incidence of SCD in China was 418.4/100,000. If calculated by the population of 1.3 billion, the total number of sudden deaths in China was about 544,000/year, ranking first in the world.
The concept of sudden cardiac death
Definition: Sudden death due to heart causes is characterized by quickness, natural and unexpected within 1 hour after symptoms occur. About the etiology of SCA, 80% are coronary heart disease, chronic myocardial scar after myocardial infarction, acute plaque instability, rupture, bleeding and thrombosis. 10-15% are cardiomyopathy, including hypertrophic cardiomyopathy and dilated cardiomyopathy. Less than 5% of uncommon causes, such as primary electrical activity and hereditary ion channel abnormality, valvular disease or congenital heart disease, and other reasons. The triggering mechanism of SCA: transient ischemia, hemodynamic fluctuation, neurocardiovascular influence and environmental factors.
Prevention and treatment of sudden cardiac death-first aid outside the hospital
First aid outside the hospital:
Timely cardiopulmonary resuscitation and electrical defibrillation;
Most patients can not get timely and effective cardiopulmonary resuscitation;
The data shows that the popularity and effect of SCD out-of-hospital first aid are not good; According to the data of the United States in 2004, there were 166,000 cases of sudden cardiac death outside the hospital. Among them, only about 60% received emergency medical services, and the average survival rate after rescue was only 6.4%.
The above data may be lower in China.
Electrical defibrillation should be performed as soon as possible for patients with sudden cardiac death. Early defibrillation is the key to improve the survival rate of cardiac arrest.
Promote the use of AED (automated external defibrillator) in public areas with relatively high probability of witness cardiac arrest. Try to shorten the interval between stopping pressing and giving electric defibrillation, and CPR must be resumed immediately after giving electric defibrillation.
In 2010, JACC magazine reported the comparison of survival rate between CPR alone and CPR+AED for SCD patients outside the hospital. 13769 cases of SCD were selected, and only CPR was given before EMS arrived, with a survival rate of 9% (382/4 403). The survival rate was 24%(69/289) after CPR+AED treatment before EMS arrived, which was more than 2 times higher. Logistic regression results show that:AED therapy was significantly related to the survival rate of SCD patients, and the OR value was 1.75(p<0.002).
Current situation of AED configuration in China
At present, the number of defibrillators installed in public places in China is very limited, and fewer people know how to use them, which makes many patients lose the opportunity of first aid. It is difficult to carry around and play a role in time. It is impossible to issue treatment before the patient has syncope, which reduces the damage of important organs.
Prevention and Treatment of Sudden Cardiac Death —— Application of Wearable Defibrillator (WCD)
WCD can monitor the heart rhythm in real time. Once a patient has ventricular fibrillation, it can identify ventricular fibrillation in the shortest time, deliver electrode defibrillation, and effectively save the patient’s life. Automatic glue spraying during defibrillation; No conductive paste, no sticky electrode sheet; Light weight (the wearing part is only 0.815 kg); Make patient’s conscious judgment before defibrillation; Bidirectional wave 150 joules; Record and save the data 30 seconds before the heart event; Store ECG data for up to 75 minutes at a time.
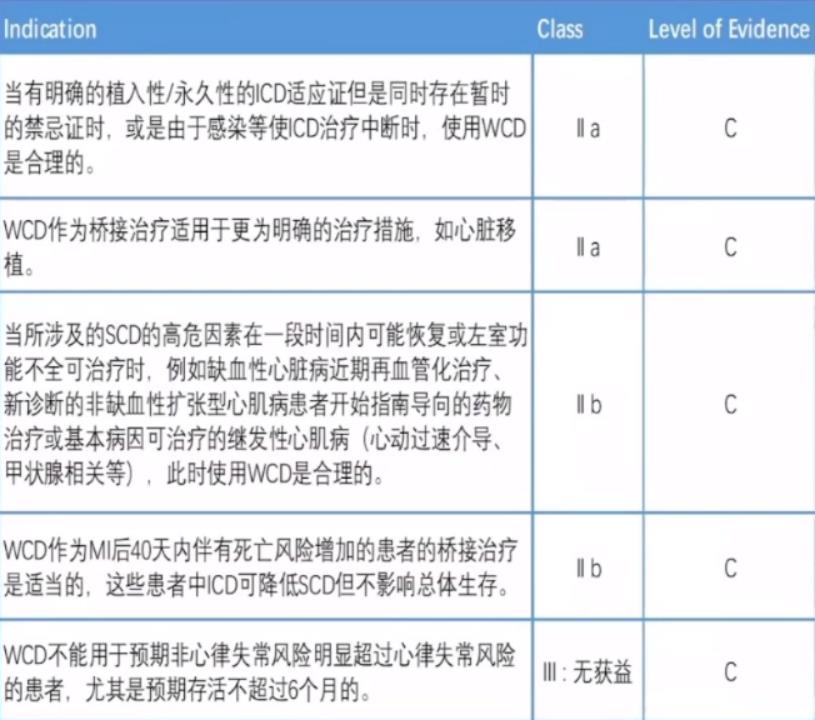
AHA medical advice:
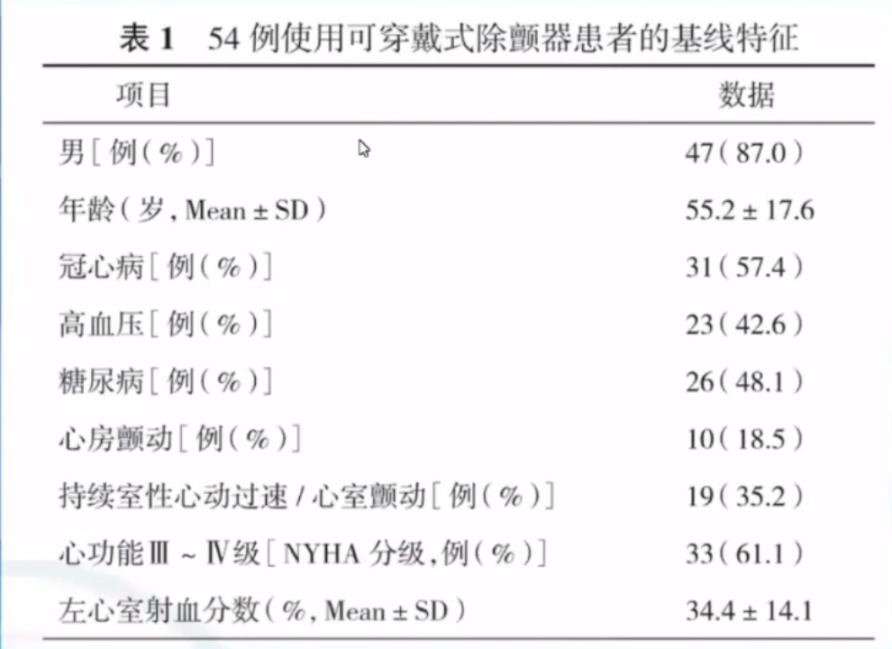
WCD technology has also been preliminarily studied in China. From June 2018 to October 2019, Fuwai Hospital and several hospitals jointly led a multi-center clinical observation study on wearable defibrillators in China. 54 patients with WCD were enrolled,Baseline information is as follows:
Indications of WCD under study:
1. Early acute myocardial infarction (within 40 days) with LVEF≤35%, 19 cases (35.2%).
2. 9 cases (16.7%) were waiting for heart transplantation and had high risk of SCD.
3. ICD could not be implanted temporarily for various reasons (such as infection), 7 cases (13.0%).
4. Newly diagnosed non-ischemic cardiomyopathy with LVEF<35%, 5 cases (9.3%).
5. Five cases (9.3%) met the secondary prevention of SCD, but the estimated survival time was less than one year.
6. ICD implantation was refused for various reasons (such as economy), 5 cases (9.3%).
7. After emergency revascularization (within 3 months), LVEF≤35%, 4 cases (7.4%).
Follow-up
1. Average wearing days: 51 34 days (longest 145 days, shortest 1 day);
2. Only 18 patients (33.3%) insisted on wearing it for one month during the three-month follow-up;
3.59.3% patients feel good about wearing; 33.3% feel ordinary when wearing;
4. The two main problems of wearing are the influence, and the size does not meet the requirements of its own body shape;
5. Only one patient was monitored for ventricular fibrillation (successful defibrillation);
6. Error-free discharge occurs.
The most effective means to prevent sudden cardiac death-implantable defibrillator (ICD)
In the United States, the annual incidence of sudden cardiac death is 250,000 to 350,000, and the average survival rate is only 5%. It is necessary to identify this high-risk patient to prevent cardiac arrest. Data show that ICD is as effective as 99% in the treatment of cardiac arrest. At the earliest, ICD needed open chest implantation, and now there are many jugular vein implants.
The progress of ICD treatment: the first ICD was implanted in the United States in 1980, approved by FDA in 1985, simple program control in 1987, hierarchical treatment in 1988, non-thoracotomy electrode lead system in 1989, biphasic ICD system in 1989, chest ICD system in 1993, unipolar defibrillation in 1993, miniaturization in 1993-1997, prolonged life and improved diagnostic ability. Now it has become a widely used method to prevent sudden cardiac death.
2017 ACC/AHA/HRS Guidelines for Patients with Ventricular Arrhythmia Management and SCD Prevention
Class I indications:
1. Survivors of SCD caused by ischemic heart disease, ventricular tachycardia or ventricular fibrillation, or stable ventricular tachycardia caused by hemodynamic instability or irreversible factors, with an estimated survival time of > 1 year, ICD implantation is recommended.
2. In patients with ischemic heart disease and syncope, if electrophysiological examination induces monomorphic sustained ventricular tachycardia and the expected survival time is more than 1 year, ICD implantation is recommended.
3. If the LVEF of ischemic heart disease is less than 35%, at least 40 days after myocardial infarction, or 90 days after revascularization, if the cardiac function is still Grade II or III on the basis of drug treatment guided by the guidelines, ICD is recommended for primary prevention.
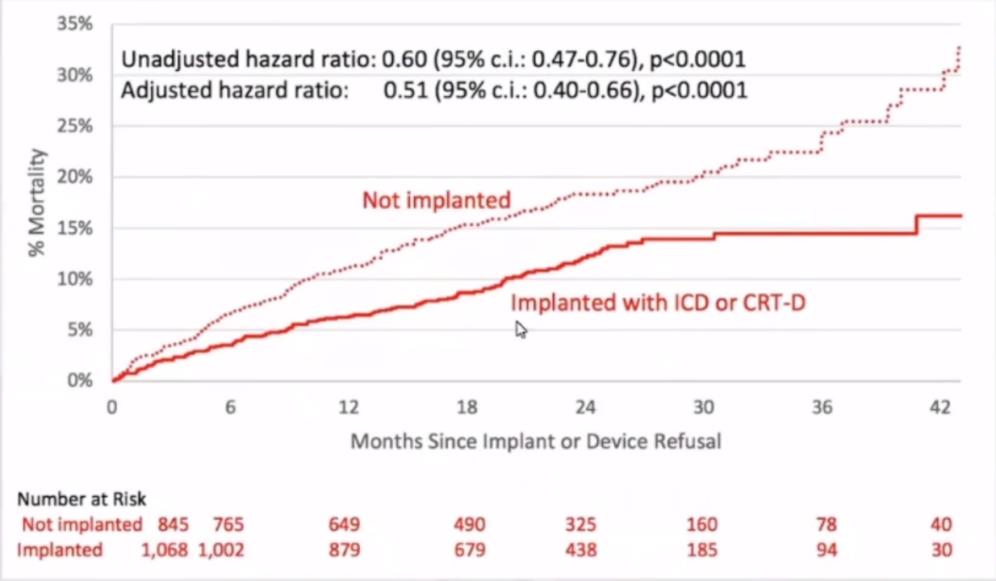
Although ICD is a type I indication, it also has defects. After ICD is implanted in human body, its utilization rate is not very high. A prospective, non-randomized international multi-center clinical study of so-called level 1.5 prevention enrolled 3889 patients in 17 countries.
Level 1.5 prevention = level 1 prevention plus one or more items:
Non-persistent ventricular tachycardia; Frequent ventricular premature beats (> 10 beats/hour); LVEF<25%; History of syncope.
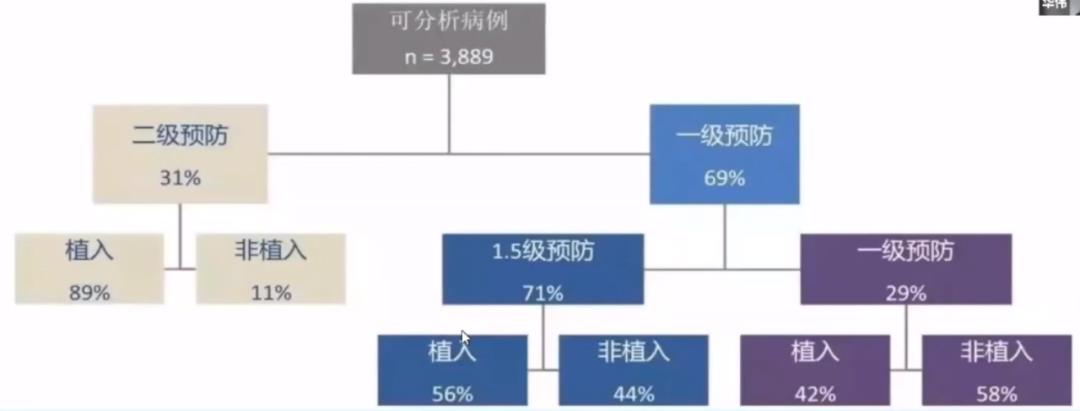
The results showed that the average follow-up was 21 10 months. Compared with the patients who did not receive ICD implantation, the all-cause mortality of the patients who received ICD implantation decreased by 49%.
The application of ICD in China, the first epicardial ICD system was implanted in 1992, and the first intravenous ICD system was implanted in China in 1996. With the formulation of ICD implantation indication guidelines and publicity and education, the number of implants has increased greatly every year since 2002. At present, about 5000-6000 patients are implanted with ICD every year in China. The proportion of primary prevention and secondary prevention in patients with ICD implantation in China is equal.
Difficulties that traditional intravenous ICD system may encounter;
Subclavian vein occlusion;
Vascular malformation;
Wear of venous lead (broken lead/broken insulation);
Difficult to pull out the lead (infection and other reasons);
The whole system needs to be removed due to infection.
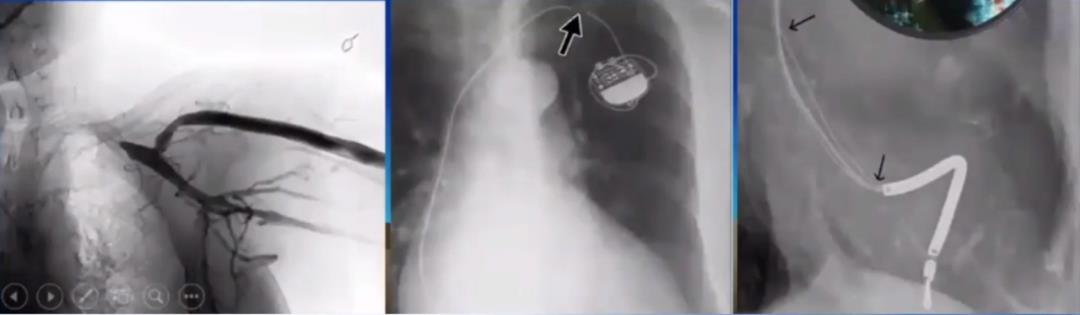
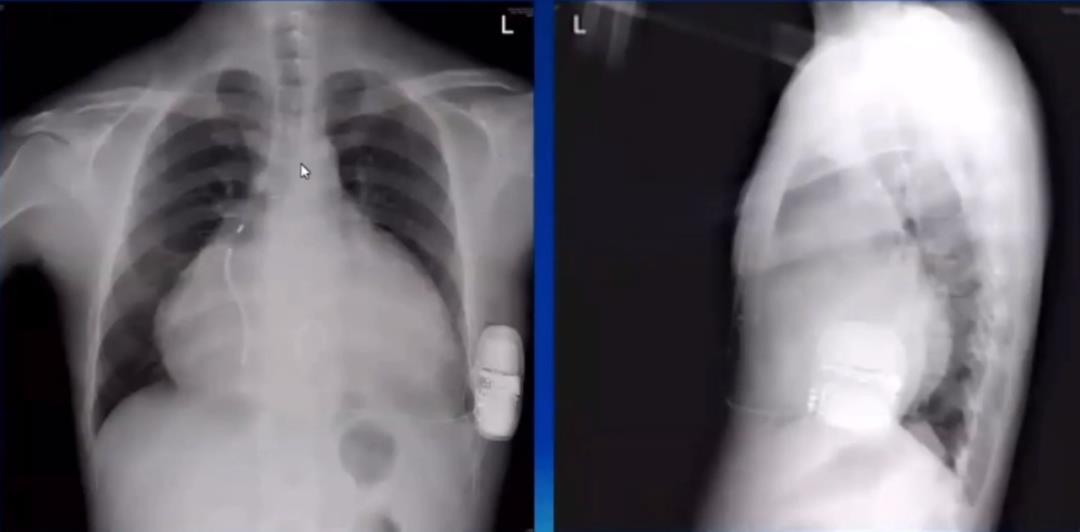
In order to reduce and avoid complications caused by defibrillation leads via intravenous ICD electrodes, a brand-new technology "total subcutaneous ICD" has been developed. Vein-free lead defibrillation system, subcutaneous implantable ICD system, total subcutaneous implantation. There is no need to implant electrode leads into the heart through blood vessels to ensure the structural integrity of blood vessels. Implantation is strictly in accordance with anatomical structure, and radioscopy is not needed during implantation. The disadvantage is that pacing is not possible.

On December 23, 2014, Fuwai Hospital implanted the first SICD in China.
In 2015, ESC Guidelines recommended its Class Ⅱa:
For patients with ICD indications who do not need pacing, CRT or ATP treatment, S-ICDs should be considered as an alternative treatment for intravenous ICD.
2017 AHA/ACC/HRS VA/SCD guidelines will transfer it to Class I indications, but there are conditions:
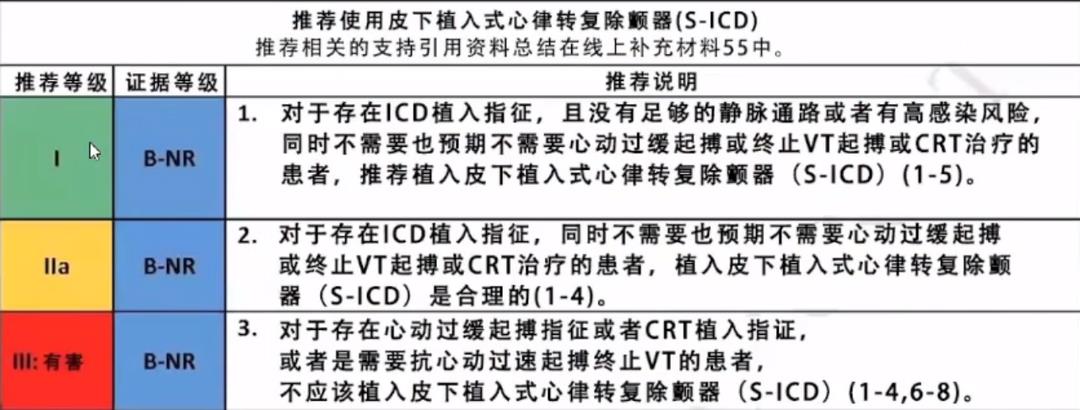
"Implanting a subcutaneous cardioverter defibrillator (S-ICD) has a lower risk of infection than TV-ICD. Therefore, S-ICD is more suitable for patients with high risk of infection, such as patients with device infection, patients with end-stage renal disease, or patients with long-term immunosuppression. "
Multi-center SICD research in China and follow-up analysis of clinical application in multi-centers in implantable cardioverter defibrillator under the skin included 111 patients who successfully implanted S-ICD in 42 centers in China and had stable follow-up. The follow-up period was (272 283) d, with 39 cases of primary prevention (35.1%) and 72 cases of secondary prevention (64.9%). The results showed that 22 patients (20.8%) received 51 appropriate defibrillation treatments, and 9 patients (8.5%) had 24 inappropriate defibrillation treatments. The main cause of inappropriate defibrillation is t-wave oversensing. It is suggested that S-ICD implantation is effective and safe in China.
NEJM magazine published a prospective randomized controlled study of PRAETORIAN. This is the first prospective randomized controlled head-to-head study of S-ICD vs TV-ICD. There are 849 patients enrolled in 39 centers (Europe and the United States) in 6 countries, including 426 cases of S-ICD and 423 cases of TV-ICD. All products of TV-ICD can be enrolled (single cavity ICD), with ICD indications and meeting the requirements of S-ICD implantation.
Main end point:Compared with TV-ICD, S-ICD has non-inferiority, inappropriate electric shock, complications related to ICD system and needing intervention, and lead-related complications.
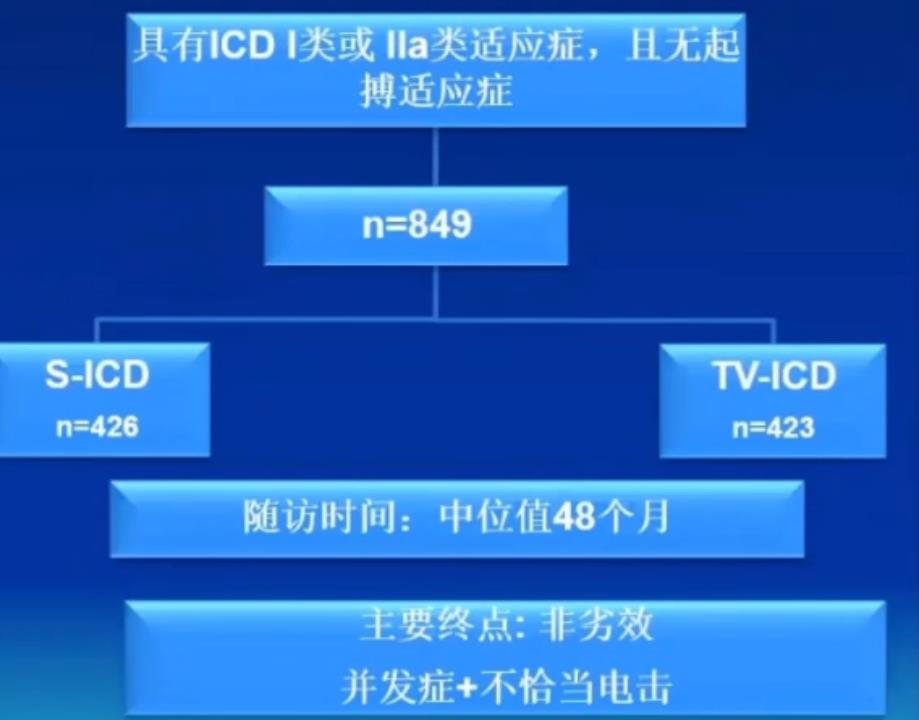
Main results:The incidence of inappropriate treatment and complications of S-ICD is similar to that of TV- ICD. The mortality of S-ICD & TV-ICD is low; The lead-related complications were significantly reduced, with 6.6% (n=24) in the control group (TV-ICD) and 6.6%(n=24) in the control group (TV-ICD).
The future and development prospect of SICD. The disadvantage of full subcutaneous ICD is that it can not effectively pace the heart. If the patient has bradycardia, he can pace bradycardia with the help of a leadless pacemaker.
Another feasible scheme, EV-ICD,Defibrillation coil is under the sternum, closer to the heart, and can conduct effective cardiac pacing. The purpose of research and development is to realize low defibrillation threshold (DFTs), small size, long service life and pacing function including ATP (anti-tachycardia pacing) through EV-ICD. This technology has been clinically studied.
EV-ICD research is a prospective, non-randomized, first long-term clinical study in human body. Patients who meet the indications of class ⅰ or ⅱ A ICD were included; Under fluoroscopy, the defibrillation lead was buried in the posterior sternum area by subcutaneous tunnel tool, and the pulse generator was placed on the left side of the chest. The defibrillation efficiency was tested by inducing fibrillation during implantation, detecting and converting ventricular fibrillation. The energy to terminate ventricular fibrillation was usually 20J once or 30J; twice in succession. Follow-up was performed at 2 weeks, 4-6 weeks and 3 months after operation. The main safety end point was no instrument or operation-related complications within 3 months after operation.
The results showed that 21 patients tried to implant, and finally 20 patients successfully implanted EV-ICD;. One patient with mediastinal fibrosis failed to be implanted successfully.
Defibrillation therapy:One patient failed to induce ventricular fibrillation/tachycardia; 89.5% patients (17/19 cases) successfully terminated ventricular fibrillation, and the defibrillation threshold was ≤30J, and the median defibrillation threshold was 15J;. The defibrillation threshold of 10.5% patients was > 30J.
Bradycardia treatment:95% patients (19/20 cases) successfully completed the pacing test, and the pacing threshold in acute phase was ≤10V, with an average of 5.1±1.9V;; R wave perception test: the average amplitude of R wave is 3.2±1.7mV;; The amplitude of R wave during ventricular fibrillation is 2.8±1.7mV, and ventricular fibrillation during operation can be correctly identified.
EV-ICD studies the clinical application experience of long-term implantation of infrasternal extravascular ICD, which proves that EV-ICD overcomes the shortcoming that SICD can’t pace, and will have a wider application prospect.
summary
Sudden cardiac death should attract our attention. The prevention and treatment of sudden cardiac death in China has a long way to go, and we need all of you to work together to reduce the occurrence of SCD in China and save more patients.
-End-